The old syphilis is back: what you need to know about “the great imitator”
Figures from the World Health Organization (WHO) warn of an increase in cases worldwide.

Share
Syphilis is not a thing of the past. While many people believe it was eradicated years ago, figures from the World Health Organization (WHO) and the current Argentine Ministry of Health warn of an increase in cases worldwide and nationally. It affects both people with penises and vulvas, and unlike other chronic STIs, it is curable.
By Alejandra Zani
Illustration: Flor Capella
“When people talk about syphilis, they think of prehistoric times, but it’s a disease that’s still around and on the rise, much more common than people realize,” Dr. Valeria Fink, an infectious disease specialist and member of the Clinical Research staff at Fundación Huésped, explained to Presentes. “It’s a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum (TP), which is primarily transmitted through sexual contact and congenitally and perinatally (through pregnancy), and it can be cured with antibiotic treatment.”
In December of last year, the Ministry of Health announced through the Bulletin on HIV, AIDS and STIs in Argentina that the rate per 100,000 inhabitants rose from 11.7 to 35.2 between 2013 and 2017, reaching a rate of 50.3 in 2018. According to this report, the most vulnerable population is that of young people aged 15 to 34, with a rate of 130 per 100,000 inhabitants.
“My first reaction when the syphilis test came back positive was ambivalent,” DG (38 years old) tells Presentes. “On the one hand, I read this information that cases are multiplying, but it still sounds like such an old sexually transmitted disease that you think it’s been overcome. When the test came back positive, I felt that it should be eradicated or under control.”
DG knew that syphilis was an STI, but she wasn't aware that it could be asymptomatic. “Perhaps I had it a long time ago, and when the test came back positive, it took me quite by surprise. My first concern was thinking about my recent sexual encounters. I notified them, and everything was fine.”
“THE GREAT SIMULATOR”
In many cases, syphilis doesn't cause symptoms, and its lesions aren't always visible. Furthermore, they often don't hurt, bleed, or itch, so patients only seek medical attention when they can see them. "This is easier for people with penises, who have visible lesions, but when the lesion is in the anus or vagina, it's often unknown," explains Sol Ferreyra ( @sol_despeinada on social media), a professor in the Department of Human Pathology at the University of Buenos Aires. "This is why it's called the great imitator in the medical world."
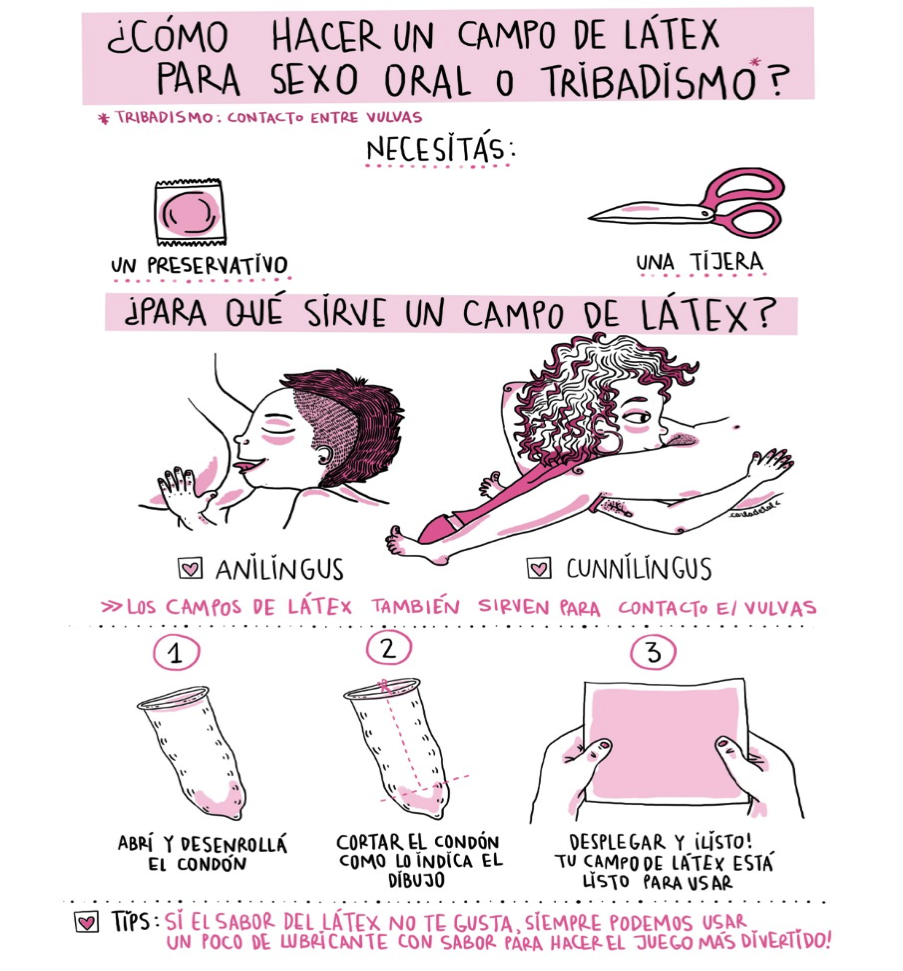
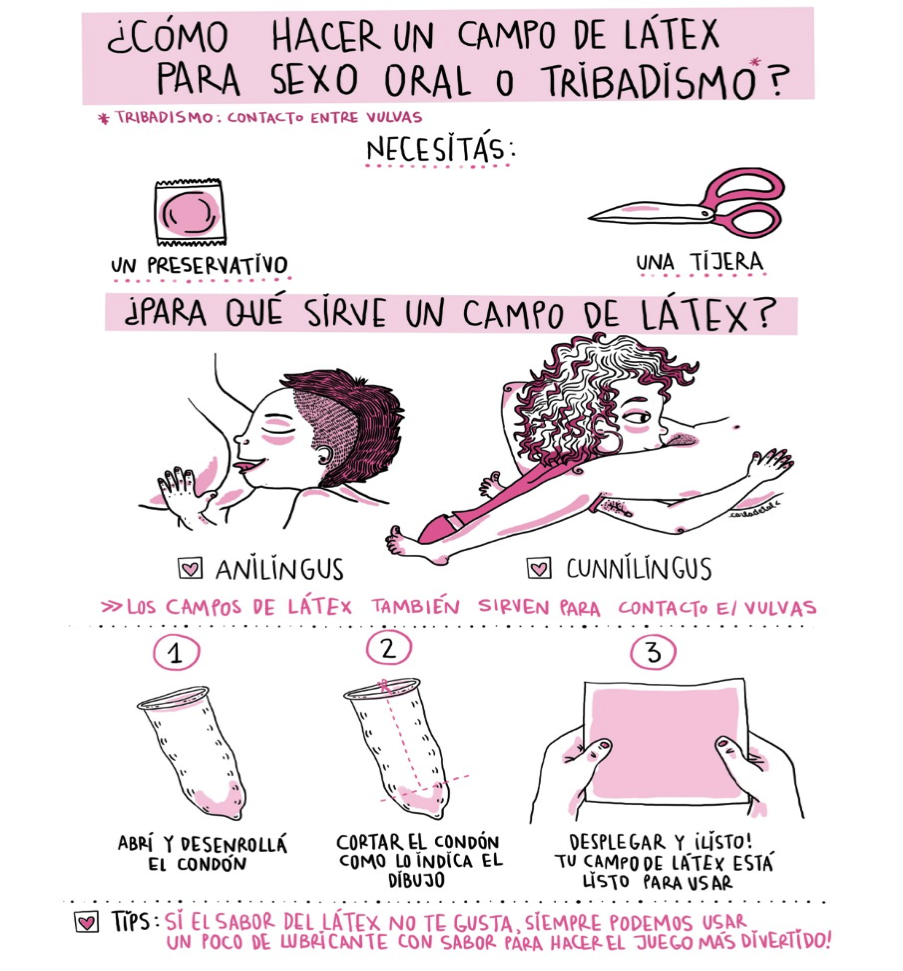
For Ferreyra, syphilis doesn't discriminate based on gender. "When it comes to transmission, anyone who is infected and has a lesion, whether it's two vulvas in contact, two penises, or a penis in contact with an anus or through the mouth, can transmit the infection," she explains to Presentes. "Sex toys can also transmit it. In this sense, the most vulnerable people are those who don't use barrier methods, such as condoms, dental dams, or latex gloves throughout the entire sexual act. There's no getting around it."
At the statistical level, the former National Ministry of Health also does not differentiate syphilis cases by transmission route. “This makes it very difficult to determine which sectors of the LGBT+ population are most vulnerable,” explains Romina Mauas, a member of the SADI AIDS and STIs Commission and medical coordinator at Helios Salud. “In the current notification form, where physicians must report syphilis cases to the government, the distribution is still by biological sex, with more women being reported than men. However, we believe this is related to cases of congenital syphilis during pregnancy, where follow-up is very thorough. Regarding cases of men who have sex with men, national statistics show that the 16-24 age group is the most vulnerable. While cases among women who have sex with women are not broken down by sex, the number of cases seen in clinics is lower.”
For Dr. Fink, the biggest problem in this regard is the lack of information. “The trans population is vulnerable in terms of access to healthcare. Many trans women engage in sex work and sometimes don't have the option of using a condom, and in addition to limitations in access to healthcare, they are also vulnerable socially. On the other hand, women who have sex with women need to know that, in the event of a lesion, they can also transmit the virus. That is to say, transmission doesn't only occur through penetration, because the chancre (the name for syphilitic lesions in their initial stage) can be located on the vulva, or it can be transmitted through oral sex.”
After the positive diagnosis, while undergoing treatment, DG reflected on how much he would have liked a more active government presence in campaigns and other initiatives. “I was treated at a privileged healthcare facility like the Fernández Hospital, which has an infectious disease department, but we know that's not the case everywhere. I wonder what it's like in other places that don't have these resources. It's not something that's being talked about, but it's happening a lot.”
DETECTION AND PREVENTION
The infectivity of sexually transmitted syphilis is highest—around 60%—in the initial stages. “At this stage, the most typical lesion is the syphilitic chancre, which can be located in the genital areas (anus, vagina, penis, vulva, and lips) as well as in the oral cavity. Over time, these ulcers may heal on their own, which does not mean that the infection has been cured,” explains Dr. Fink. “After some time, secondary syphilis can appear, which is like an outbreak on the body that can affect the torso, legs, face, or, typically, the appearance of rashes on the palms of the hands and soles of the feet. When this happens, many people think it's an allergic reaction, but it's syphilis. The important thing is to consult a doctor and have blood tests done to obtain a timely diagnosis.”
This was the case for AR (29 years old). “When I found out I had syphilis, I was shocked. I assumed it was an allergic reaction I often have to stress, just a bit more severe and with rashes on my vulva. I knew very little about this disease; I thought it was a thing of the past, and I would have liked to know immediately that it is a curable disease,” she tells Presentes.
While it has been said that one of the main reasons for the rise in syphilis cases is the decrease in condom use, Dr. Fink cautions that there is no single, absolute cause that determines the reason for the outbreak. “Because HIV has been brought under control in patients who adhere to their treatment, achieving an undetectable viral load and therefore making the virus untransmissible, the use of protective methods has decreased. And if you look at the statistics from the National Directorate of AIDS and STIs, new cases are appearing among men who have sex with men, but this is not the only cause.”
For Mauas, changes in people's sexual behavior, coupled with the increase in sexual encounters through mobile apps, are also indicators of rising STIs among young people. “This is because social transformations haven't been accompanied by greater sexual and reproductive education from the government, or at least not as much as we would like,” she tells Presentes. “The use of pre-exposure prophylaxis (PrEP) has reduced fear of HIV, but that doesn't mean other STIs can't be transmitted. There is a lack of information on comprehensive sexuality education and budget cuts for sexual and reproductive health services.”
Check the map of fixed condom distribution points here.
HOW IS SYPHILIS CURED?
For AR, the positive diagnosis was a shock. “I questioned who I had sex with, why I hadn't used protection, and I was afraid it was a chronic illness. This was due to my own lack of knowledge. I didn't know it was curable. Luckily, the gynecologist informed me that it would be curable with injections, and that I should notify the people I had had sexual relations with so they could get tested and stop the transmission.”
While specialists affirm that the best prevention comes from using barrier methods, even these don't guarantee complete protection. "Syphilis can be transmitted even when using a condom correctly because there can be lesions outside the condom's coverage," explains Mauas. "What's important to know is that it's curable with antibiotic treatment. Although it's a very old infection, the microorganism hasn't developed resistance to penicillin, so this is the treatment of choice. It's administered by injection, and the number of doses is determined according to the stage of the infection."
For those who cannot receive penicillin, the SADI researcher states that alternative treatments or lower doses are available. “After 48-72 hours of application, a response to the treatment begins. But even if cured, syphilis does not leave protective antibodies. You can be cured, but if you are re-exposed, you can contract syphilis every time you are exposed, and this is quite high in the early stages of infection. That's why we always recommend using barrier methods.”
CONGENITAL SYPHILIS
Syphilis can also be transmitted perinatally, that is, from mother to child. In these cases, it is called congenital syphilis. “The number of women who contract syphilis during pregnancy is increasing. If there is no early detection and timely treatment, or if the treatment cannot be administered properly, the child will be born with congenital syphilis, which can lead to low birth weight and other complications, if not pregnancy loss,” explains Mauas.
“Pregnant women are a particularly vulnerable population, and all should be tested for syphilis at least once per trimester of pregnancy,” adds Dr. Fink. “The risk is that the baby could be born with very serious birth defects if the woman contracts syphilis during pregnancy and it is not treated. These are the cases we absolutely must report, and they are what is most concerning.”
According to the specialist, this situation shouldn't be happening, since by law women should have a check-up once per trimester, as indicated on their prenatal care card. She also points out that it is part of the State's and the Directorate of AIDS and STIs' role, as a representative body, to "ensure the free provision and distribution of condoms in numerous health centers." She further warned that, in terms of prevention, they are always "one step behind."
“We know there were some shortages, but in general, condoms are available. People can go to health centers and get condoms and lubricants. It's important to use water-based gel and avoid saliva and other creams, as saliva can also spread other STIs.”
We are present
We are committed to journalism that delves into the territories and conducts thorough investigations, combined with new technologies and narrative formats. We want the protagonists, their stories, and their struggles to be present.
SUPPORT US
FOLLOW US
Related notes
We are present
This and other stories are not usually on the media agenda. Together we can bring them to light.





